PRS (Pierre Robin Sequence)
Ian McLain and His Story of Being Born with Pierre Robin Sequence
On
November 15, 2011, Ian McLain was born, along with his twin brother
Ryan at approximately 34 weeks of gestation. Their mom, Liz, had
experienced an uneventful pregnancy (as much as a twin pregnancy can be)
and no abnormalities had been detected in any of the tests (quad
screen, ultrasounds). While Ryan suffered from some complications of
prematurity, his condition was relatively good. However, Ian was born
with a birth defect known as Pierre Robin Sequence. Pierre Robin
Sequence (PRS) is the name given to a combination of birth defects which
usually include a small lower jaw, cleft palate and a tendency for the
tongue to "ball up" in the back of the mouth. Many of these children
have breathing and feeding problems early in their lives. Each child can
be affected differently. For the next 8 weeks, Ian would spend his
life in the NICU’s in two different states, and his immediate and
extended family would be on an emotional roller coaster of hope and
fear. The end result, however, is an extremely positive one that we
would like to share with the world. It is our hope that Ian’s story and
the information below will be of help to families with children born
with PRS, and that their story can have as happy of an ending as ours
has so far. If you find this page useful or want to send me a comment
or question please use my "Contact Me" page.



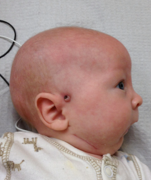
Ian
was born via caesarian at 7:30AM on 11/15/2011. Just after his birth
(as Baby B), we heard a faint cry, but then not much more. Liz and I
were a bit worried, and I was constantly watching the nurses and trying
to reassure her that everything was ok. The nurses brought Ian over so
Liz and I could see him (and get the picture), and informed us that he
had a cleft palate. Much to our concern, as soon as we were able to take
this picture, the nurses called for respiration to come up stat. While
we were worried about the need for additional procedures, we were
assured that everything was ok.

Both Ian and Ryan were taken to the hospital’s NICU shortly after birth
and it was about an hour before I was allowed to go down and see them.
Upon arrival, I saw that Ryan was doing well, but that Ian was on
several machines and had an endotracheal tube inserted and was receiving
additional oxygen and breathing help. I was told that due to the
caesarian delivery, his lungs still had some fluid in them, but that
everything else was fine. We were very relieved when we came to visit
the next morning and found that the endotracheal tube had been removed.

After several days and a lot of time under the UV lights to raise their
bilirubin scores, we were told that a geneticist had been called in to
evaluate Ian. We were caught off guard by this and asked why.
Originally, all we were told was that he had a partial cleft and some
trouble breathing. After talking with the neonatologist, we were told
that they though he might have PRS, but they did not give us any
information beyond the possible diagnosis. Liz and I immediately
started doing research, and our first stop was https://pierrerobin.org/This is a great site for learning about PRS, and we soaked up as much information as we could
Days eventually turned into weeks. We continued to learn more about
PRS, and learned more about how to read the monitoring machines than I
think we had ever wanted to know. Because of their physical features,
PRS babies often suffer from breathing difficulties, because their
airway is blocked by their own tongue. As a result, a major issue to
watch for in a PRS baby is his/her blood oxygen saturation and how it
correlates with the heart rate. A “dsat”, referring to a desaturation
of oxygen in the blood, is when the blood oxygen level drops (monitors
will generally be set to notify the nurse if the saturation drops below
85%) and is correlated with a drop in the heart rate. These dsats are
an indication that the airway is blocked. If not handled quickly (by
giving supplemental oxygen and making sure the airway is cleared) this
can lead to potential brain damage and/or death. Even if your baby is
not being monitored, a dsat can be noted by the presence of a blue tinge
around the baby’s lips and nail bed.
Things for Ian seemed to be going well. He was breathing on his own and
was eating some of his feedings from a bottle with a little bit of
help. He was in a crib side by side with Ryan, and we were allowed to
hold him whenever we wanted. Ryan went home on December 7th, and we
started to get excited about the possibility of having both boys home
for Christmas.

Unfortunately, this optimism did not last. It was only a few days later
that we found out that Ian had apparently aspirated some of the breast
milk during one of his bottle feedings and had developed a black spot in
one of his lungs, indicating pneumonia. All of the progress he had
made was gone, and we were back to seeing him naked on an emergency bed,
needing breathing support, and receiving his nutrition via either an
i.v. or a feeding tube. We were devastated. He was now having up to 7
dsats a day and the neonatologist mentioned the possibility of a gastric
tube (gtube) for feeding and a tracheostomy. Both of these were things
that we really did not want to hear, and moreover, were things we did
not want to have to put Ian through. We knew there had to be a better
way.


It
is necessary to provide some background information on me and Liz at
this point. Liz, my wonderful wife, was the first person on either side
of her family to go to college, and earned a PhD from the University of
Alabama at Birmingham in Pharmacology/ Toxicology. I am a computer geek
with a background of making the impossible happen on a regular basis.
Neither
one of us has a “it’s not possible” attitude, and as such, never take
what people tell us at face value. I should also mention that my mother
is an MD, and as an intern did work with cleft pallet patients. Over
the last 25+ years, she and my father (also a physician) have been
running a symposium about Rheumatology for doctors, and my mother has
become increasingly interested in research. The reason I mention this
is that it was her research on PubMed (www.pubmed.org) that eventually turned up the miracle we had been looking for.

Liz and I had decided that we did not want Ian to have to come home with
a trach or a gtube, and considered that these were signs of failure.
We were going to do everything we could to
make sure he would come home as healthy and appartus-free as possible.
If you read through the Pierre Robin Network website on the procedures
that are currently being performed for mandibular (jaw) distraction,
it is clear that there are a lot of options, most of them requiring
multiple surgeries, and having extensive lists of potential
complications. We knew we didn’t want Ian to have to go through any
more surgeries than necessary, so for us, the use of a bioresorbable
device was highly attractive. However, the question was who could do it,
and how soon could they do it? There are doctors all over the US who
will do these surgeries, and there is even one in Birmingham who can do
them, however, most of them will not even see the child until they are 6
months of age - for us, that just wasn’t acceptable.
Our lives at this point were pretty much in overdrive. It had been 4
weeks since Ian and Ryan were born, Thanksgiving had passed, and we were
both working from home and taking care of our 2 1/2-year-old, Simon,
and Ryan. Everyday we would make 2 trips to the hospital to see Ian.
One was Liz going with either her parents or both of our mothers, and
the second was me going by myself or with my parents. We were looking
for signs that Ian was getting better. Some days he seemed to be making
progress, but he seemed to have reached a plateau in how well he was
doing. His weight fluctuated up and down by a few ounces, but was never
on a true uphill gain. He was off the oxygen, but was still hooked up
to a nasal cannula blowing air into his nose to help keep his airway
open. Moreover, he was still mostly being fed via an NG tube.

It was on one of these trips that my mother told Liz and I that she had
found a group in Seattle that could do the surgery on Ian. We were
ecstatic. In one day our whole outlook had turned around. We now had
proof that a solution was out there. Two days later, my mother came
back and said that she had found a second group that could do the
surgery, and that they were doing them on children as young as 7 days
old and had a 98% success rate. The group was in Atlanta, less than a 3
hour drive, and she wanted to know if we wanted her to do a write up
and get in contact with them. We jumped on the possibility immediately,
and she sent an email off the clinic the next day with a full medical
write-up of Ian. A few days later (Tuesday), she got an email back from
Dr. Fernando Burstein, M.D. and he wanted to have Ian transferred to
Childrens Hospital at Scottish Rite in Atlanta the next day, and perform
surgery on Thursday. We got in touch with his office and immediately
started making plans. Everything else was on hold.
Now, Liz and I have health insurance through the company that I work for
that is backed by Blue Cross and Blue Shield (BCBS) of Alabama. BCBS
had been very good to us up to this point. We saw the case worker at
the NICU several times and really didn’t have any concerns about them
covering the transportation or surgery. We had the neonatologist sign
off on Ian’s transport, and from everything we were hearing, the
transfer was a go. On Wednesday we called the NICU in Birmingham for a
status update, and on their side, everything was on track. They said
they were waiting to hear back from Scottish Rite and that it would most
likely be the afternoon before he was moved. Sometime around noon we
got a call from our BCBS case worker that the transport had been denied
because there was a doctor in Birmingham who could perform the surgery.
We were furious. Didn’t they understand the difference that another 4
months would make? Not to mention that Ian would have to receive the
trach in order to come home before the surgery. We submitted all of the
papers that Burstein’s group had been publishing and made sure they
understood that there was a dramatic age gap between when the groups
would perform the surgeries. The data then had to go before a review
panel and they would not give us any indication of how long that review
would last or when we would hear back. All we could do is sit back and
wait. Not being one to do that, I kept calling people.
Not 2 hours later, I got a call from our BCBS case worker. They had
approved Ian’s transport and everything was a go. I just about fell
into tears and thanked her for all the help.

Scottish Rite took care of everything. Four hours later, Ian was picked
up via ambulance with a respiratory therapist and nurse on board (we
were not allowed to ride with him), and a little over 3 hours later, he
was in the Children’s Hospital of Atlanta (CHOA) NICU.

The whole time we were working with BCBS we had been packing and
planning where we were going to stay. Having our 2 1/2-year-old son and
1-month-old Ryan along for the ride, we
knew we wanted a hotel room with 2 bedrooms. There is a Staybridge
Suites just a few miles from CHOA that has 2 bedroom suites and a
discount for those staying for a long period of time. In our case, we
were planning for 12 days based on our discussion with the Burstein
group. We booked our room, packed our minivan, and headed to Atlanta.
It was late before we got to our hotel room and got everyone unloaded. Liz stayed with Simon and Ryan, and I headed over to Scottish Rite to check on Ian and fill out the remaining paperwork. When I got there (and got through security - whew!) I found Ian sleeping the most peacefully I had seen him sleep since he was born. The nurses were awesome (the RN’s have a 3 to 1 maximum patient to nurse ratio ) and each NICU pod has a dedicated NP and respiratory therapist. The difference between this NICU and the one he had left in Birmingham was dramatic, although there were many caring and skilled nurses working at the NICU in Birmingham, they were overworked and plagued by budgetary issues. As I started talking to his nurse that night, I was absolutely stunned when she asked me a very simple question. What took you so long to get him here?
It was late before we got to our hotel room and got everyone unloaded. Liz stayed with Simon and Ryan, and I headed over to Scottish Rite to check on Ian and fill out the remaining paperwork. When I got there (and got through security - whew!) I found Ian sleeping the most peacefully I had seen him sleep since he was born. The nurses were awesome (the RN’s have a 3 to 1 maximum patient to nurse ratio ) and each NICU pod has a dedicated NP and respiratory therapist. The difference between this NICU and the one he had left in Birmingham was dramatic, although there were many caring and skilled nurses working at the NICU in Birmingham, they were overworked and plagued by budgetary issues. As I started talking to his nurse that night, I was absolutely stunned when she asked me a very simple question. What took you so long to get him here?
She wasn’t referring to the ambulance ride or working with the insurance
company. No, to her, getting a 5-week-old baby in for this surgery was
OLD. It was at that point that I knew we had made the right choice,
and that Ian was in the right place.

To our surprise, both of my parents had decided to reschedule all of
their patients and come to Atlanta with us to help out. So the next
morning, we left the little ones with them and headed to see Ian before
his surgery. We walked with him down to the surgery area, met Dr.
Burstein for the first time as he explained the procedure to us, signed
all of the paperwork, and
went back to the waiting room to sit and wait. They told us it could
take up to 2 hours for the surgery, so I went out to the hallway and
took a quick conference call for work. Less than an hour later, I
turned around and saw Dr. Burstein coming down the hallway. He gave me a
big thumbs up and said everything went perfectly and that Ian was in
recovery. I thanked him, excused myself off the call, and headed
straight to Liz (who apparently had already talked with Dr. Burstein).
We thought it was especially nice of Dr. Burstein to come tell us the
outcome of the surgery himself. It would be 20 minutes before Ian would
come back from recovery, and the nurses stopped at the waiting room to
let us see him before they took him back to the NICU. It was about 20
more minutes after that before we were allowed to go back into the NICU
to see him.
The procedure that Dr. Burstein’s team performs is to make a small
incision on each side of the face and to cut the jaw just below the
joint. Then, they attach the bioresorbable distractor and insert screws
that will help spread apart the cut in the jaw, allowing it to be
lengthened. Ian’s jaw was moved forward 5 mm during surgery, and he was
given two days to heal. After that, they re-evaluated him. Since
everything looked good, they proceeded to move the jaw forward 1 mm
twice a day until the target position was reached. With Ian, this took 7
days, and his jaw was moved an additional 15 mm, for a total of 20 mm
(slightly less than an inch). The difference, even immediately after
surgery, was astounding.
As
soon as we saw Ian for the first time after surgery, we could tell that
it had been a success. For one, he was on his back and NOT having
breathing issues. You have no idea what a relief that was. Something
we had not previously known, but that we found out from Dr. Burstein
after surgery, was that Ian was “tongue-tied”. Being tongue-tied is a
birth defect in which the tongue does not fully disjoin from the base of
the mouth. It is a very simple procedure to fix the problem, however,
it was Dr. Burstein’s belief that his being tongue-tied was the reason
he had made it so long without a trach. The tied frenulum kept his
tongue from falling back into his airway, allowing him to breathe almost
normally in certain positions (such as on his stomach).
In
total, we ended up being in Atlanta for 19 days. During that time, Ian
continued to get better and slowly started to gain weight. He was
finally on the right track, and Liz and I were extremely excited.

12/22/11

12/23/11

12/24/11

12/25/11

12/26/11

12/27/11

12/28/11

12/29/11

12/30/11

12/31/11

01/01/12

01/05/12

01/08/12

01/09/12

01/12/12
Since he was discharged on January 9th, Ian has been doing well and
gaining weight. We were sent home with a feeding pump, NG tube
placement training, and an apnea monitor. The monitor is on him most of
the day - especially if we are working or he is sleeping. However, he
pulled out his NG tube the 3rd day he was home. We had not used it
since bringing him home, so we decided to leave it out and see what he
could do with the bottle. We had been using the Haberman
nipple (now also referred to as a Special Needs Feeder) with Ian since
his surgery at Scottish Rite, and continue to use it at home. He is now
taking over 80ml per feeding by bottle and we have never had to use the
feeding pump. He has also gained almost 2 lb since coming home, and
although we have to take his monitor with us everywhere we go, has been
out to eat and shopping with us without a problem.
Advice
If you remember back to the question the nurse asked me when I first
arrived at Scottish Rite, you will get the idea of why Liz and I wanted
to create this site. Time and information are key, and it can be
difficult to make decisions when you first discover that your child is
diagnosed with PRS. Like to so many other parents out there, we wanted
to share our story and the information we have learned so that we can
potentially help another family who is contemplating whether their child
should receive a trach, and whether there is any hope for their child
to have a normal life. Below are a few tips based on our experiences:
- If the NICU you are in does not have experience with PRS, you need to take action. Either transfer your child to a NICU that does, or do your best to instruct the nurses to help them learn. The difference between a NICU that deals with PRS babies and one that doesn’t is dramatic.
- The NICU may try to get you out fast for insurance reasons and out of a misguided desire to allow you to have your child come home as soon as possible - DO NOT LET THEM SEND YOU HOME. PRS babies need special attention and rushing their discharge will only set them back and frustrate you.
- Most hospitals - especially Children’s of Atlanta - have Ronald McDonald houses and arrangements with local hotels. Be sure to ask before you make your arrangements, because you can save a lot of money if you are going to be there a while.
- READ READ READ and READ some more. The more informed you are as a parent, the faster and easier it will be to make decisions on things that pop up.
- Be sure to have a support group of some kind. Had it not been for the grandparents on both sides, I doubt Liz and I would have made it through this with our sanity. Almost 3 weeks in a hotel with 2 children and 1 in the hospital is trying, to say the least.
Helpful Links
- Pierre Robin Network
- Childrens Healthcare of Atlanta Pediatric Hospital
- Pediatric Plastic Surgery & Craniofacial Associates
Update (2012)
On January 31, 2012 - Liz, Ryan, and I made the journey back to
Atlanta. This time we were destined for Dr. Burstein’s office, where
Ian was to have his screws removed. The process was extremely quick,
and took only 5 minutes to complete. It will be three more months
before we can have his cleft palate repaired, but at the rate he’s
growing and with the progress he is making, that is something we don’t
mind waiting for.

Left Side
Right Side

